Spinal Hernia Treatment at Sanus Axis clinic in Vilnius
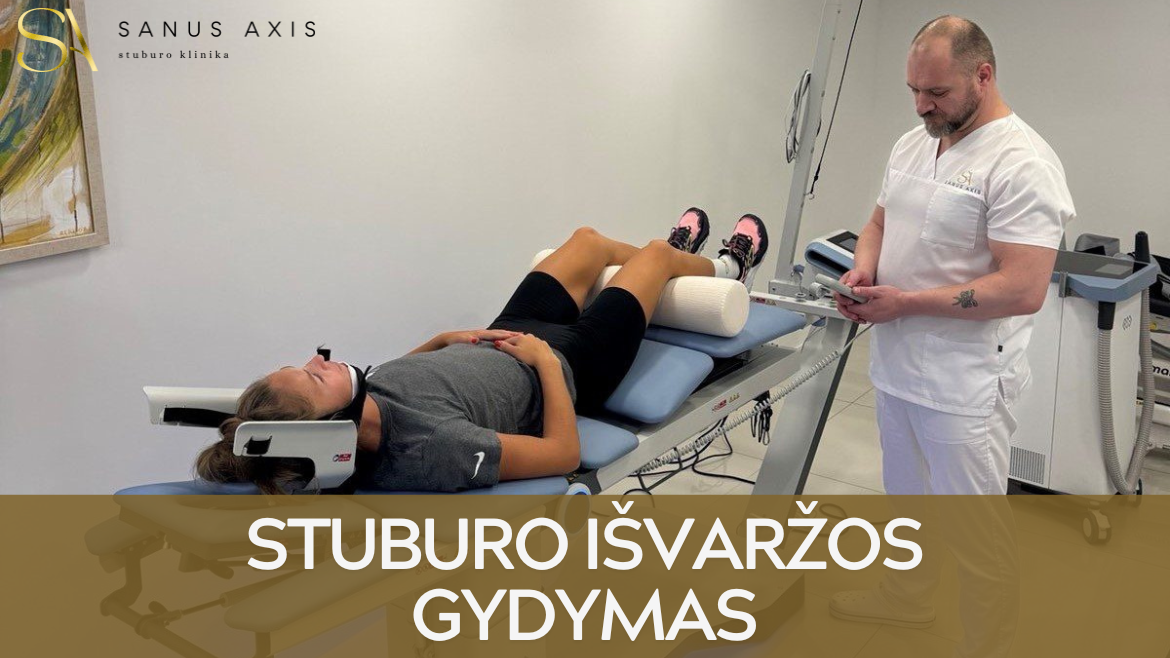
Private clinic Sanus Axis specializes in treating spine and musculoskeletal disorders.
Our manual therapy and physiotherapy specialists use evidence-based methods that target the root cause of pain and help patients avoid surgery.
Each patient receives an individualized treatment plan based on biomechanical diagnostics and a thorough assessment of spinal function.
Why Patients Choose Sanus Axis:
- The clinic employs highly qualified manual therapy and physiotherapy specialists;
- We use advanced medical equipment not available elsewhere in Lithuania;
- Treatment combines manual therapy, spinal decompression, physiotherapy, and nerve mobilization to restore natural spinal biomechanics;
- The average treatment course is only 5 sessions, after which patients return to normal activity.
What Is a Spinal Hernia?
Spinal Hernia occurs when part of an intervertebral disc shifts out of place and compresses nearby spinal nerves.
This change causes back, neck, or limb pain, muscle weakness, numbness, and restricted movement.
A spinal disc hernia most often develops in the lumbar or cervical region due to poor posture, physical strain, or disc degeneration.
Timely treatment helps patients avoid surgery and fully restore mobility
Causes and Risk Factors of Spinal Hernia
The vast majority of patients who come to our clinic seek help for limb, back, or even head pain, numbness, or aching caused by a spinal hernia. The bad news is that in some cases a spinal hernia cannot be cured even with surgery, but the good news is that it is absolutely possible to live without pain or discomfort, says Sanus Axis manual therapy specialist Sergii Ratushnyi.
He notes that many patients have already tried numerous treatment methods or are even considering surgery before visiting the clinic. It often happens that even after successful surgery, the hernia returns after some time, the specialist explains.
A spinal hernia most commonly forms in the lumbar region (about 60%) and the cervical region (about 40% of the time). These conditions cause back, neck, or limb pain, numbness, and movement limitations.
The number of hernias keeps increasing because most people spend the majority of the day sitting. The pandemic left a strong mark — people realized they could work without leaving home, and movement decreased even further. Long hours spent at computers or smart devices significantly affect posture and spinal stability, Ratushnyi adds.
Poor nutrition, excess weight, low physical activity, and genetic factors also contribute to spinal hernia development.
One of the most frequent causes is age-related disc degeneration. As intervertebral discs lose elasticity over time, they become more prone to cracking or compressing, which raises the risk of herniation.
Common Patient Mistake – Self-Treatment
One of the most common mistakes that worsens back health is self-treatment.
After learning they have a hernia, some people start exercising excessively and choose exercises that are not appropriate, causing more harm than good. This is why I always recommend consulting specialists instead of trying to treat the condition on your own, emphasizes Sanus Axis manual therapy specialist Sergii Ratushnyi.
Unsupervised massage, excessive physical load, or poor posture can worsen the hernia and trigger inflammation.
Effective spinal hernia treatment requires accurate biomechanical diagnostics and a personalized therapy plan.
Sanus Axis specialists identify the cause of the hernia and use non-invasive treatment methods that address the root problem rather than only relieving pain.
Stages of Spinal Hernia
A spinal hernia develops gradually as the intervertebral disc loses elasticity and its inner material begins to press on nearby nerve structures.
Each stage has distinct characteristics and requires a tailored treatment approach. Early diagnosis often prevents the need for surgery.
| Stage | Description | Key Symptoms | Treatment Approach |
|---|---|---|---|
| Protrusion | The soft disc nucleus shifts outward but remains inside the disc. | Mild back aching, tension, stiffness after sitting or physical strain. | Conservative treatment – physiotherapy, posture correction, manual therapy. |
| Prolapse | The nucleus pushes against the outer edge of the disc, increasing pressure on nerves. | Back pain radiating into the limbs, feeling of instability. | Personalized physiotherapy program, decompression therapy, physiotherapy modalities. |
| Extrusion | The disc ring tears, and part of the nucleus protrudes into the spinal canal. | Sharp pain, numbness, muscle weakness, postural changes. | Intensive non-surgical treatment, nerve mobilization; in some cases surgery. |
| Sequestration | A fragment of the nucleus fully separates from the disc and compresses nerves in the spinal canal. | Severe pain, limb numbness, impaired bladder or bowel control. | Urgent medical care – surgery and rehabilitation are often required. |
Symptoms of Spinal Hernia
Symptoms depend on the hernia’s location, size, and whether spinal nerves are compressed.
Pain
- A lumbar hernia causes lower back pain that radiates into the buttocks, legs, or feet (radiculopathy).radikulopatija);
- A cervical hernia causes neck pain that radiates into the shoulders, arms, or fingers.
Sensory Changes
- Numbness, tingling, or burning sensations appear in the affected area.
- Reflexes may weaken, and sensitivity may decrease.
Muscle Weakness
- Compressed nerves lead to weakness in the arms or legs.
- Walking, lifting objects, or maintaining balance becomes difficult.
Pain Intensification
- Pain increases after physical activity or prolonged sitting or standing.
- When the hernia significantly compresses nerves or the spinal canal, urinary or bowel dysfunction and numbness in the lower limbs may occur — this requires urgent medical attention.
Spinal Hernia Diagnostics
At Sanus Axis, diagnostics are performed comprehensively — assessing both imaging and functional data to identify the true cause of the hernia, not just its effects.
The diagnostic process includes:
- MRI and X-ray imaging – used to precisely identify disc damage, nerve compression, and inflammation.
- Biomechanical spine assessment – a detailed posture, muscle balance, and movement analysis that reveals overloaded areas of the spine.
- Neurological and functional load tests – evaluation of reflexes, muscle strength, mobility, and pain responses.
- Consultation with a physiotherapist, during which an individualized diagnostic and treatment plan is created.
This thorough approach allows specialists to accurately determine which spinal segment is affected, which nerve is irritated, and which therapy will be most effective.
Rehabilitation After Spinal Hernia Treatment
Rehabilitation after spinal hernia treatment is essential for restoring spinal stability, muscle strength, and balanced movement.
Whether the treatment was non-surgical or surgical, the body needs time to adapt to new biomechanical conditions and recover the function of affected tissues.
Rehabilitation Goals
- Restore muscle strength and balance around the spine to reduce nerve compression and the risk of hernia recurrence.
- Improve range of motion and coordination so the patient can safely return to daily activities.
- Reduce remaining pain or tension using physiotherapy and stretching techniques.
- Strengthen posture and ergonomic habits that help prevent future spinal overload.
Rehabilitation Process
In the early stage, immediately after treatment, light isometric and stabilization exercises activate deep muscles and improve circulation.
Later, exercises become more dynamic with increased load and movement range until full mobility is regained.
Additional physiotherapy methods, such as electrical stimulation or heat therapy, may be used to accelerate tissue healing.
In the final phase, the patient learns safe movement patterns, proper lifting techniques, and correct sitting posture to prevent relapse.
Rehabilitation Duration
The duration depends on the type of hernia, the treatment method, and the patient’s physical condition. On average, non-surgical recovery takes 4–6 weeks, while post-surgical rehabilitation may last up to 12 weeks or longer.
A properly managed rehabilitation process enables full functional recovery and a return to normal, pain-free life.
When to See a Specialist
You should consult a spine specialist if back, neck, or limb pain does not improve within a few days and begins to limit movement.
A specialist evaluation is necessary if:
- Pain radiates into the legs or arms, or you experience tingling, numbness, or burning sensations.
- You feel muscle weakness or have difficulty maintaining balance.
- Pain increases when sitting, standing, or bending, even after rest.
- You feel stiffness in the morning or after long periods of sitting.
- You experience urinary or bowel dysfunction — this may indicate severe nerve compression and requires urgent medical attention.
- Pain persists for more than 1–2 weeks despite medication or massage.
The earlier a spinal hernia is diagnosed, the higher the likelihood of successful non-surgical treatment.
Spinal Hernia Prevention
Proper spine care, regular physical activity, and correct movement patterns help maintain healthy intervertebral discs and prevent degeneration.
- Maintain good posture. Avoid slouching while sitting or standing. When working at a computer, keep the monitor at eye level and your feet firmly on the floor.
- Move regularly. Spend at least 30 minutes per day on physical activity such as walking, swimming, or light stretching and stabilization exercises.
- Strengthen deep core muscles. Strong abdominal, pelvic, and back muscles support spinal stability and reduce disc load.
- Avoid sudden movements and improper lifting. When lifting objects, bend at the knees instead of the waist and keep the load close to your body.
- Manage body weight and nutrition. A balanced diet, sufficient hydration, and healthy body weight reduce the risk of disc degeneration.
- Optimize workplace ergonomics. Use an adjustable desk, suitable chair, and take breaks every 45–60 minutes.
- Reduce stress. Tension affects muscle tone and can intensify pain, making emotional balance important for spinal health.
Frequently Asked Questions (F.A.Q.)
How long does spinal hernia treatment take?
Treatment duration depends on the hernia stage and the patient’s overall condition.
On average, 4–6 sessions at Sanus Axis are enough for patients to experience significant improvement and return to normal activity.
Can a spinal hernia heal without surgery?
Yes. About 80–90% of spinal hernias are successfully treated with non-surgical methods such as physiotherapy, manual therapy, and decompression.
Surgery is needed only in complex cases involving severe nerve compression.
Can a spinal hernia recur?
Yes, especially if the underlying causes — postural imbalance or muscle weakness — are not addressed.
Proper rehabilitation and individually selected stabilization exercises reduce recurrence risk significantly.
Does physiotherapy help if the pain is severe?
Yes. Even with strong pain, physiotherapy can reduce inflammation, relieve nerve compression, and improve blood flow.
Exercise intensity is adjusted to the patient’s condition, ensuring safe and gradual progress.
When should I seek urgent medical care?
If pain radiates into the legs or arms, or if numbness, muscle weakness, or urinary and bowel dysfunction appear, seek immediate medical attention.
These symptoms indicate severe nerve compression and require urgent evaluation.